Abstract
Introduction
The majority of secondary central nervous system (CNS) lymphoma cases are derived from histologically high-grade systemic lymphomas such as diffuse-large B cell lymphoma (DLBCL) and Burkitt's lymphoma. These CNS lymphomas are associated with poor prognosis and a low likelihood of long-term survival, especially rituximab-ineffective CD20- lymphoma. To investigate the biological features and potential therapeutic targets of CNS-involved CD20- lymphoma, we established the first known patient-derived xenograft (PDX) model using cerebrospinal fluid (CSF).
Methods
Six- to 8-week-old male NSG mice (Jackson Laboratory) were housed and monitored in our animal research facility. All experimental procedures and protocols were approved by the Institutional Animal Care and Use Committee of The University of Texas MD Anderson Cancer Center. A total of 0.08 million cells were isolated from 2 mL of CSF obtained from a CD20- CD79A- DLBCL patient with Bcl-2 and Myc rearrangements (double-hit). The isolated cells were directly injected into a human fetal bone chip implanted into NSG (NSG-hu) mice. After passage, the mice were administered several small molecules, and tumor burden was measured via tumor volume and human β2M levels over the course of treatment. Kaplan-Meier survival analysis was also performed. PDX tissue was collected for histological analysis, immunophenotyping, genotyping, and proteomics analysis.
Results
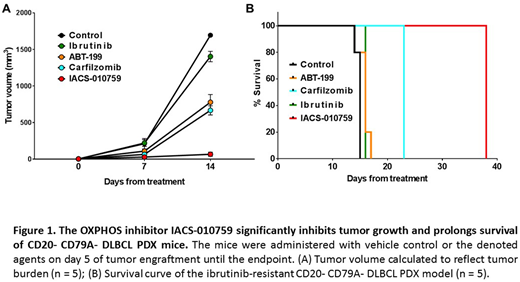
The PDX tumors possessed the same histological, genetic and immunophenotypical features as the primary patient tumor cells. The PDXs had Bcl-2 and Myc rearrangements and were positive for CD10, CD19, CD22, and CD45 and were negative for CD5, CD20, and CD79A. After tumor passage, the mice were treated with vehicle, 50 mg/kg ibrutinib (Bruton's tyrosine kinase (BTK) inhibitor) oral gavage daily, 50 mg/kg ABT199 (Bcl-2 inhibitor) oral gavage daily, 1 mg/kg carfilzomib (proteasome inhibitor) i.v. twice per week, or 7.5 mg/kg IACS-010759 (oxidative phosphorylation (OXPHOS) inhibitor) oral gavage daily. As shown in Figure 1, the PDX tumor was resistant to the BTK inhibitor ibrutinib and moderately responsive to the proteasome inhibitor carfilzomib. Although the Bcl-2 gene was rearranged, the PDX model only had a partial response to the Bcl-2 inhibitor ABT-199 (ABT-199 vs control, p = 0.0004). In contrast, inhibition of the OXPHOS pathway with IACS-010759 significantly inhibited 96% tumor growth (IACS-010759 vs control, p < 0.00001) and prolonged mouse survival by approximately 25 days compared with the vehicle control and the other drugs (IACS-010759 vs control, ABT-199, or ibrutinib, p < 0.0001). Moreover, proteomics analysis demonstrated that IACS-010759 not only inhibited OXPHOS but also upregulated the pro-apoptotic protein Bim.
Conclusion
To our knowledge, this is the first PDX model generated from the CSF of a CD20- double-hit DLBCL patient. With this PDX model, we determined that the OXPHOS inhibitor IACS-010759 is a promising therapeutic agent for this aggressive cancer.
Wang:Acerta Pharma: Honoraria, Research Funding; Kite Pharma: Research Funding; Novartis: Research Funding; Pharmacyclics: Honoraria, Research Funding; Dava Oncology: Honoraria; Juno: Research Funding; MoreHealth: Consultancy; Celgene: Honoraria, Membership on an entity's Board of Directors or advisory committees, Research Funding; AstraZeneca: Consultancy, Research Funding; Janssen: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees, Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal